The Rio Rancho (NM) Fire Rescue Experience
Overview
Out-of-hospital cardiac arrest (OHCA) resuscitation focuses first on early defibrillation and high-quality chest compressions, though oxygenation and ventilation remain an integral part of patient management. An ongoing challenge with ventilation during cardiac arrest is the potential for positive pressure to adversely impact already compromised venous return. Thus, the effect of ventilation in the cardiac arrest patient has been a topic of interest and controversy for some time. Interestingly, Aufderheide and colleagues demonstrated worsening coronary perfusion pressures with increasing ventilation rates back in 2004.1
Fortunately, it does not require large ventilation volumes to create ventilation-perfusion matching in such a low flow state: low volumes match low flows. As a result, the American Heart Association (AHA) recommends 10 asynchronous breaths per minute for adults with a tidal volume of 6 to 7 cc/kg.2,3 They also provide a specific caution to “avoid delivering excessive ventilation during CPR because doing so can compromise venous return and cardiac output and decrease cerebral blood flow by causing vasoconstriction.”2
Related: Optimal Prehospital Airway Management Depends on EMS System Efficiency
Multiple studies, as well as plentiful clinical experience have revealed how challenging it is for even highly trained personnel to deliver these recommended ventilation rates and volumes. In some studies, ventilation rates were over 40 breaths per minute in adults1,4 four times the recommended standard of care. Whereas ventilation volumes are more difficult to quantify, a real-world study from 2007 did demonstrate larger than suggested tidal volume delivery.4 The cause of this overventilation is likely multifactorial in the midst of a cardiac arrest resuscitation. To combat this all too common scenario, some have even suggested using pediatric size self-inflating bags in adult resuscitative efforts.5
Another challenge for OHCA resuscitation in many EMS systems is sufficient personnel. If resuscitation is being managed by a team of only two or three providers, dedicating one person to ventilation is a real drain on resources.
One creative solution to these issues is to deploy a mechanical ventilator – assuring controlled ventilation rates and volumes as well as freeing up a provider for other lifesaving interventions. Ventilators have generally been considered contraindicated during CPR due to concerns about chest compressions causing high pressure vent alarms and potentially not delivering breaths when appropriate. This concern should have been somewhat put to rest as asynchronous ventilations are now routinely recommended once an airway is in place and have been shown to improve chest compression fraction.2,6
Despite this, ventilator use during prehospital or in-hospital cardiac arrest remains very rare in our experience. In fact, it is common teaching to remove a patient from the ventilator should they lose pulses. This axiom was intended to help troubleshoot the causes of cardiac arrest in a patient already on a ventilator, rather than to serve as a prohibition against ventilator use in these circumstances.
Unbeknownst to many EMS providers, educators and medical directors, two studies have previously reported on ventilator use during OHCA. In 1995, Johannigman et al. reported on the use of a ventilator for cardiac arrest and in 2005 Weiss et al. reported on 12 prehospital OHCA patients managed with a ventilator.7,8. A recent editorial also called for more ventilator use in OHCA.9
System Integration
In 2014, Rio Rancho (NM) Fire Rescue introduced the ParaPAC® into our cardiac arrest algorithm as seen in our treatment guidelines. (Figure 1).
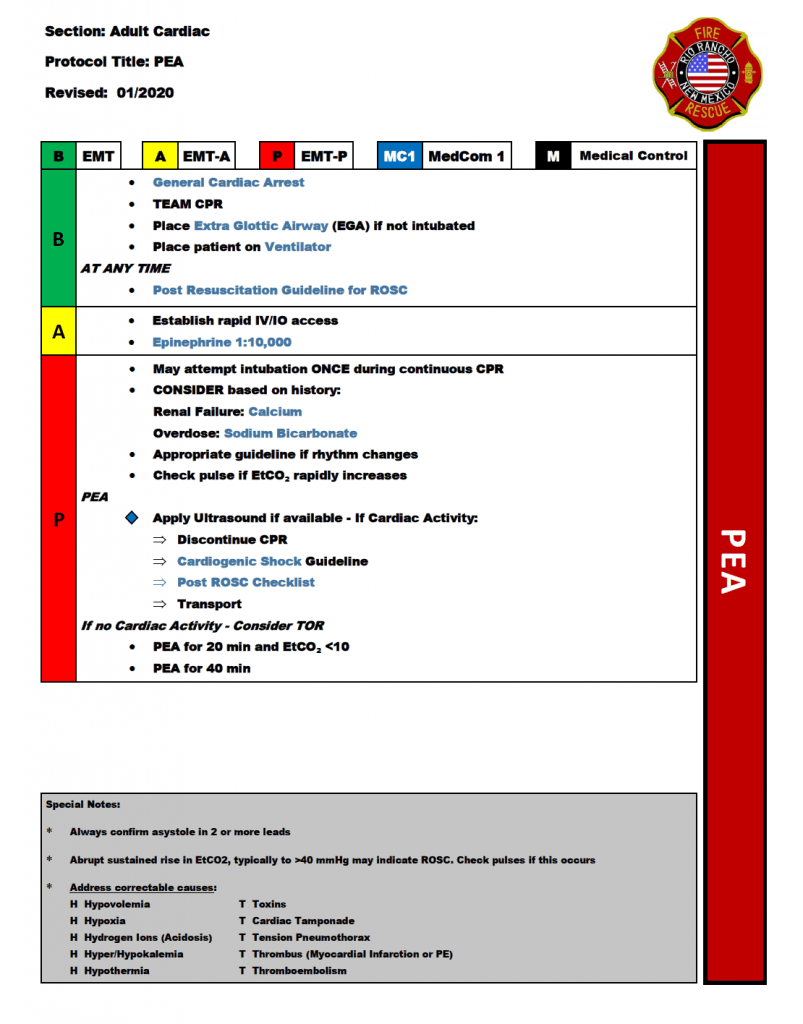
Figure 1: Cardiac arrest treatment guideline (PEA)
This was intended to both conserve personnel resources and better control ventilation. Crews are encouraged to deploy the ventilator as soon as they begin mask ventilation, and when an extraglottic device (EGD) or endotracheal tube (ETT) is inserted. Our neighbors in the City of Albuquerque (NM) Fire Rescue as well as Albuquerque (NM) Ambulance Service have also incorporated a ventilator into their cardiac arrest algorithms.
Related: It’s About Paramedic Intubation Skill Maintenance, Not ETI vs. SGA
Our department has found the ventilator simple to deploy and useful in optimizing airway management of arrest resuscitation. Our standardized approach to ventilation rates and volumes are shown in Figure 2.
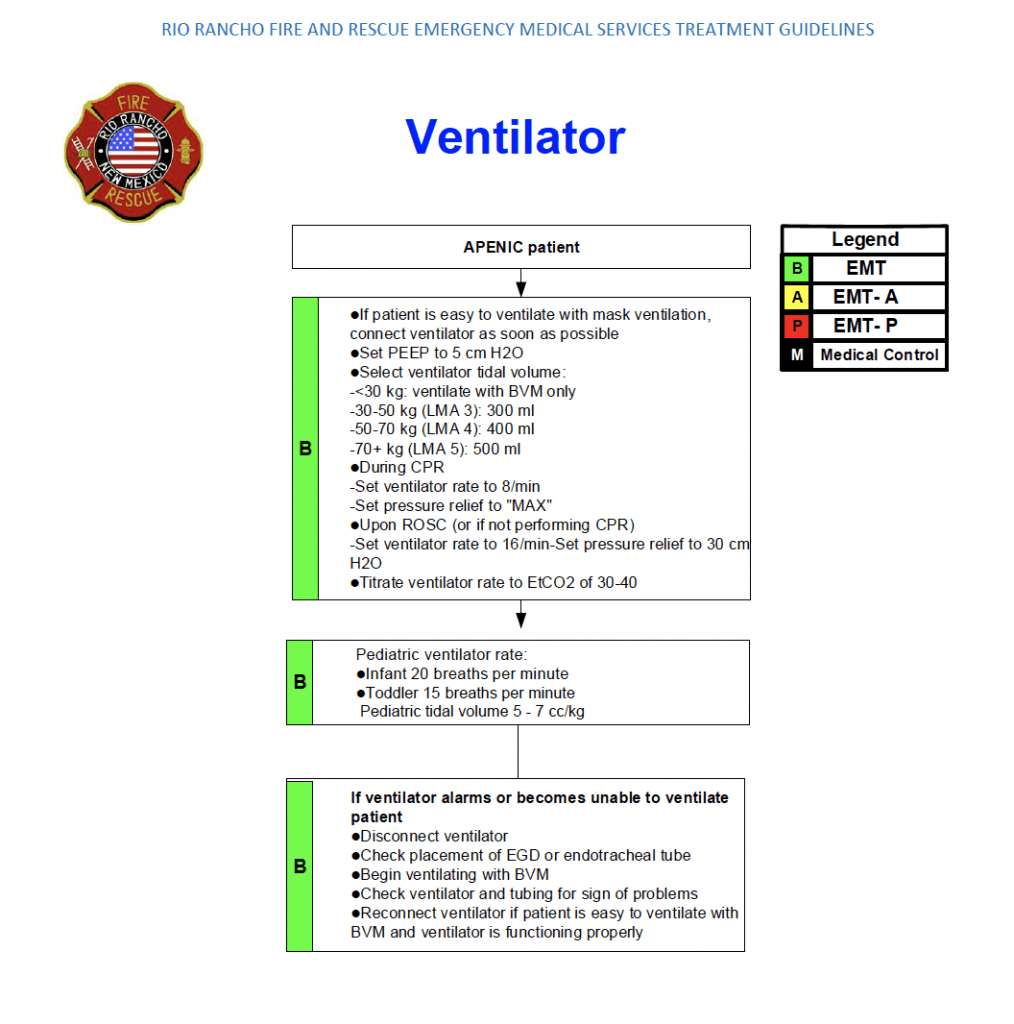
Figure 2: Ventilator procedure
These rates were based on our best interpretation of the evidence to provide ventilation-perfusion matching and avoid hemodynamic compromise, while also allowing for compensation of metabolic acidosis once return of spontaneous circulation (ROSC) is obtained. Other agencies and medical directors could potentially make the case for slightly different numbers.
For OHCA resuscitation, a complex transport ventilator is not required. Simple ventilators such as the ParaPAC® allow for easy deployment, operation and training. If ROSC is achieved after an advanced airway is placed and the patient begins to breathe spontaneously, it is possible that they will not tolerate the simple modes used on the ParaPAC® and similar ventilators. If local guidelines allow for sedation and/or analgesia administration, this may help with patient comfort. In some situations, it may be necessary to remove the patient from the ventilator and assist ventilations manually or even remove the advanced airway altogether.
Related: Prehospital Management of Difficult Airways
Training has been quite straightforward. When the ventilators were first introduced, the medical director provided in-person training sessions for as many personnel as possible. This included a 30-minute didactic session on the reasons for ventilator use and specifics about the device. This was followed by a 30-minute hands-on sessions to get familiar with the set-up, controls, and then mock codes. New personnel are trained on the device in their station with occasional formal review at scheduled continuing education sessions.
We have been fortunate to be able to place ventilators on all six of our front-line paramedic ambulances. They have been utilized on over 200 cardiac arrests since introduced and are currently deployed in approximately 80% of cases. (Figure 3).

Figure 3: Image of the ParaPAC in use
Use has increased over time as we have placed more ventilators into service and as providers have become more familiar with using them. We also found that placing the ventilator in the bag with other airway equipment was more effective than having a separate bag that did not always make it from the truck to the bedside. The most common reason they are not utilized during an arrest is when there are unclear advanced directives and crews are trying to sort out a patient’s wishes while performing only basic life support interventions.
We are currently working to evaluate and summarize our clinical experiences in greater quantitative detail. Given the successful utilization of these ventilators in some of our neurologically intact OHCA survivors we believe it is safe to continue their use until more data is available.
References
- Aufderheide TP, Sigurdsson G, Pirrallo RG, Yannopoulos D et al. Ventilation-induced hypotension during cardiopulmonary resuscitation. Circulation 2004;109(16):1960-5.
- Panchal AR, Berg KM, Hirsch KG, Kudenchuk PJ et al. 2019 American Heart Association Focused Update on Advanced Cardiac Life Support: use of Advanced Airways, Vasopressors, and extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest. Circulation 2019.
- American Heart Association. Part 3: Adult Basic Life Support. Circulation 2000;102 suppl 1;22-59
- O’Neill JF, Deakin CD. Do we hyperventilate patients? Resuscitation 2007;73(1):82-5
- Kroll M, Das J, Siegler J. Can altering grip technique and bag size optimize volume delivered with bag-valve-mask by Emergency Medical Service providers? Prehosp Emerg Care 2019;23(2):210-14.
- Sanson G, Ristagno G, Caggegi GD, Patsoura A et al. Impact of ‘synchronous’ and ‘asynchronous’ CPR modality on quality bundles and outcome in out-of-hospital cardiac arrest patients. Intern Emerg Med 2019;14(7):1129-37
- Johanigmann JA, Branson RD, Johnson DJ, Davis Jr K, Hurst JM. Out-of-hospital ventilation: bag-valve device vs. transport ventilator. Acad Emerg Med 1995;2:719-24.
- Weiss SJ, Ernst AA, Jones R, Ong M et al. Automatic Transport Ventilator Versus Bag Valve in the EMS Setting: A Prospective, Randomized Trial. South Med J 2005;98(10):970-976.
- McMullan J and Braude D. Poison, Pixie Dust and Prehospital Airway Management (In Press). Invited Editorial. Academic Emerg Med 2020.
Chief, Division of Prehospital, Austere and Disaster Medicine Professor of Emergency Medicine, EMS and Anesthesiology, The University of New Mexico Health Sciences Center
Assistant Professor, Emergency Medicine
Associate Director, Prehospital and Disaster Medicine
University Hospitals, Case Western Reserve University School of Medicine
Lieutenant R. Elliott Guinn is a critical care paramedic and has been involved in EMS for over 20 years. He has been with the Rio Rancho Fire Rescue for the past 14 years and is currently assigned as a senior “Medcom,” a small specially trained paramedic program responding to high acuity calls to over 100,000 people.
Rio Rancho Fire Rescue
Battalion Chief EMS Division
EMT-P
Rio Rancho Fire Rescue
Captain EMS Training
EMT-B





Dear Darren,
Great article about mechanical ventilation!
Our ventilator called MEDUMAT Easy CPR would meet your needs perfectly. Not only during CPR. Even in the course of RSI this ventilator can be easily integrated in the process.
Modes: IPPV, Demand Flow Mode, Manual Mode (through a Button called MEDUtrigger located directly at the ventilation mask).
Adjustable pressure limits for tube and mask ventilation.
Easy to use – one single knop for setting tidal volume an ventilation rate.
For any questions please feel free to reach out to me.
Kind regards,
Enrico
We have been using mechanical ventilation during OOHCA for more than 6 years now. It is an invaluable tool to control rate and vT not to mention freeing up hands. We have also reduced our respiratory rate in an attempt to decrease the VQ mismatch.