An antique item is perceived as having value because of its historical significance and is often defined as being at least 100 years old. The 1500 mL Bag-Valve-Mask Manual Resuscitator (BVM) is not that old and is probably best described as a piece of vintage ventilation equipment. Although the device still works as designed, is still in service and being used by well-intentioned clinicians, it should be on the shelf with the Medical Anti-Shock Trousers, LifePak 5 and Biophone. While change is sometimes slow, and healthcare providers can be described as conservatively fixed, lung protective ventilation is the current standard of care.
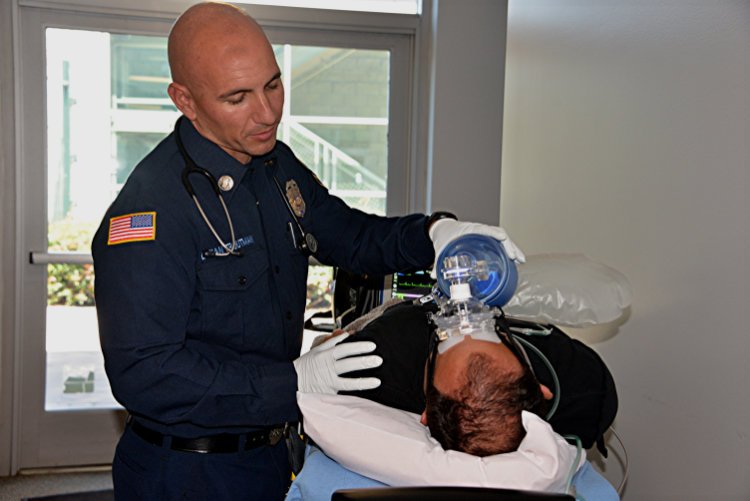
Photo by Rick McClure
A Bag-Valve-Mask Manual Resuscitator is used on a patient. The author argues the device should be put on the shelf.
There has been a considerable number of lectures and papers written in the last few years regarding ventilation rates and pressures when providing manual ventilation with a BVM. Adding pressure manometers and timing lights to a BVM is starting to become common practice. Most providers are aware the standard for ventilation rate has been reduced to 10 per minute during cardiac arrest with an advanced airway. Many providers understand that high pressure can cause barotrauma (injury from high pressure) and prefer to use a BVM with an integrated manometer. There is very little discussion, however, on the ventilation volume and the potential for volutrauma (injury from over stretching of lung tissue), even though it appears to be changing.
Recently, during a ventilation training session, I overheard a physician refer to the BVM as “The Bag of Death.” It is an interesting description for a medical professional and for a basic tool of an EMS clinician. The concept of the BVM dates to the 1950s where there is little reference to the size of the bag. When I first learned about manual ventilation in the 1970s, we were taught to squeeze the bag flat. If a comparison is made between a BVM and being ventilated by a ventilator in the 1970s, the standard was to calculate the tidal volume at 10 to 12 mL per kg. If you had a 100 kg patient, the tidal volume would be between 1,000 to 1,200 mL to support having a BVM the size of the current adult bag.
Current guidelines from the American Heart Association recommend five to seven mL per kg (500 to 700 mL for the same 100 kg patient), or roughly half as much. If so, why is the vintage 1,500 to 1,600 mL bag still in use? At the 2017 EMS Today JEMS Conference and Exposition in Charlotte, North Carolina, I was teaching manual ventilation in the hands-on experience lab. I set up a test lung with a computer that displayed volumes and pressures and asked each attending clinician to ventilate the test lung with a standard adult size BVM of 1,500 mL. What the experiment demonstrated was out of over 200 EMS responders taking the challenge, not one ventilated with the proper volume and pressure. Next, I had each clinician repeat the test using a 1,000 mL small adult bag. They were instructed to use the same technique only with a smaller bag and nearly all of the participants were able to ventilate properly. This simple change with no additional training improved one of medicine’s most fundamental skills.
What’s the harm with too much volume? High inspiratory lung volumes (or pressures) can cause injury through alveolar overdistension, causing alveolar rupture, and cell death. Second, because of an increase in transpulmonary pressure, the patient’s blood pressure can be reduced due to a reduction in pre-load. Third, the extra volume can cause gastric insufflation, creating a greater risk of aspiration.
The question now is: Which one of these side effects is acceptable to you?
In a study by Kane, it was reported that lung protective ventilation (LPV) reduces morbidity and mortality, and EMS professionals over-ventilated using an adult size BVM2. LPV is often used with mechanical ventilation where the peak airway pressure is kept below 30 cmH2O and tidal volumes are based on predicted body weight, not actual body weight. This type of ventilation has been shown to reduce ventilator-associated lung injury. Research has shown that the same type of injury can be caused during manual ventilation with a BVM.
To practice LPV:
- Limit the tidal volume by using a small adult bag (1,000 mL)
- Limit end-inspiratory pressure by using a manometer
- Provide adequate PEEP to keep the lungs open and prevent alveolar collapse
- Use a timing device to maintain the appropriate rate
What is holding back the change? The evidence is clear, and the cost is minimal. Evaluate what you are using and make simple changes for better outcomes.
- Hallett, S. and Ashurst, J. (2019). Physiology, Tidal Volume. [online] Ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/books/NBK482502/#_article-30194_s9_ [Accessed 25 Jun. 2019].
- Kane, E., Siegler, J., & Hafez, Z. (2019). Assessing tidal volumes delivered by an adult and pediatric BVMs when using chest rise as anend-point. Retrieved from www.itrauma.org/wp-content/uploads/2018/11/2-Comparing-Tidal-Volumes-Delivered-by-Adult-and-Pediatric-BVMs-When-EMS-Use-Chest-Rise-as-an-End-Point-for-Ventilation-Erin-Kane.pdf.
- Nehme, Z., & Boyle, M. J. (2009). Smaller self-inflating bags produce greater guideline consistent ventilation in simulated cardiopulmonary resuscitation. BMC Emergency Medicine, 9(1). doi:10.1186/1471-227x-9-4.
Steven C. LeCroy, MA, CRT, EMT-P, is a retired captain/paramedic from St. Petersburg Fire & Rescue, an adjunct instructor at St. Petersburg College and a 40-year respiratory therapist. He has also been an expert witness in over 100 EMS cases across the U.S.


Since the comments are now closed on your blog (lecroyemsvision.com/2019/07/26/bag-valve-mask-tidal-volume-and-lung-protective-ventilation-strategies/), I wanted to briefly reply here. The spec sheet you reference is out-dated and posted to our corporate website, Ambu.com. The correct/current specs can be found on our spec sheet posted to AmbuUSA.com, which can been downloaded that here: http://www.ambuusa.com/products/airway-management/resuscitators/product/ambu-spur-ii. The correct bag volumes for the SPUR II resuscitator (adult/pediatric/infant) are 1475 mL/635 mL/220mL.
I’ve contacted our corporate product manager and asked her to update this ASAP. Thank you for pointing out this error.
The volume of the BVM itself doesn’t take into account the smaller stroke volumes delivered, either by one hand or by two hands. These volumes are significantly lower than the volume of the device itself, by design, and one handed stroke volumes available from a 1500mL BVM satisfy the latest ventilation strategies. Also, it is better to make higher volumes available and not need them than need them but not have them available (how many of us drive vehicles that are capable of going faster than the posted legal speed limit?). This comes with proper training and clinical experience in… Read more »